Page 109 - Advances in Biomechanics and Tissue Regeneration
P. 109
6.3 ACTIVE BIOMECHANICAL BEHAVIOR 105
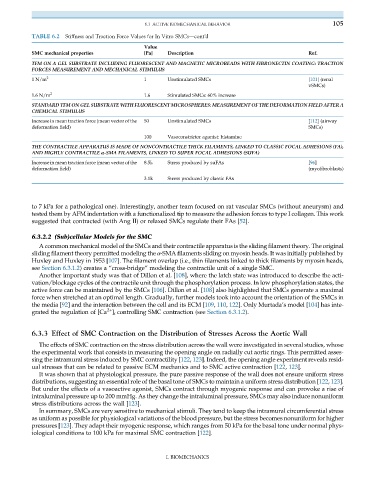
TABLE 6.2 Stiffness and Traction Force Values for In Vitro SMCs—cont’d
Value
SMC mechanical properties [Pa] Description Ref.
TFM ON A GEL SUBSTRATE INCLUDING FLUORESCENT AND MAGNETIC MICROBEADS WITH FIBRONECTIN COATING: TRACTION
FORCES MEASUREMENT AND MECHANICAL STIMULUS
1 N/m 2 1 Unstimulated SMCs [101] (renal
vSMCs)
1.6 N/m 2 1.6 Stimulated SMCs: 60% increase
STANDARD TFM ON GEL SUBSTRATE WITH FLUORESCENT MICROSPHERES: MEASUREMENT OF THE DEFORMATION FIELD AFTER A
CHEMICAL STIMULUS
Increase in mean traction force (mean vector of the 50 Unstimulated SMCs [112] (airway
deformation field) SMCs)
100 Vasoconstrictor agonist: histamine
THE CONTRACTILE APPARATUS IS MADE OF NONCONTRACTILE THICK FILAMENTS, LINKED TO CLASSIC FOCAL ADHESIONS (FA),
AND HIGHLY CONTRACTILE α-SMA FILAMENTS, LINKED TO SUPER FOCAL ADHESIONS (SUFA)
Increase in mean traction force (mean vector of the 8.5k Stress produced by suFAs [96]
deformation field) (myofibroblasts)
3.1k Stress produced by classic FAs
to 7 kPa for a pathological one). Interestingly, another team focused on rat vascular SMCs (without aneurysm) and
tested them by AFM indentation with a functionalized tip to measure the adhesion forces to type I collagen. This work
suggested that contracted (with Ang II) or relaxed SMCs regulate their FAs [52].
6.3.2.2 (Sub)cellular Models for the SMC
A common mechanical model of the SMCs and their contractile apparatus is the sliding filament theory. The original
sliding filament theory permitted modeling the α-SMA filaments sliding on myosin heads. It was initially published by
Huxley and Huxley in 1953 [107]. The filament overlap (i.e., thin filaments linked to thick filaments by myosin heads,
see Section 6.3.1.2) creates a “cross-bridge” modeling the contractile unit of a single SMC.
Another important study was that of Dillon et al. [108], where the latch state was introduced to describe the acti-
vation/blockage cycles of the contractile unit through the phosphorylation process. In low phosphorylation states, the
active force can be maintained by the SMCs [106]. Dillon et al. [108] also highlighted that SMCs generate a maximal
force when stretched at an optimal length. Gradually, further models took into account the orientation of the SMCs in
the media [92] and the interaction between the cell and its ECM [109, 110, 122]. Only Murtada’s model [104] has inte-
2+
grated the regulation of [Ca ] i controlling SMC contraction (see Section 6.3.1.2).
6.3.3 Effect of SMC Contraction on the Distribution of Stresses Across the Aortic Wall
The effects of SMC contraction on the stress distribution across the wall were investigated in several studies, whose
the experimental work that consists in measuring the opening angle on radially cut aortic rings. This permitted asses-
sing the intramural stress induced by SMC contractility [122, 123]. Indeed, the opening angle experiment reveals resid-
ual stresses that can be related to passive ECM mechanics and to SMC active contraction [122, 123].
It was shown that at physiological pressure, the pure passive response of the wall does not ensure uniform stress
distributions, suggesting an essential role of the basal tone of SMCs to maintain a uniform stress distribution [122, 123].
But under the effects of a vasoactive agonist, SMCs contract through myogenic response and can provoke a rise of
intraluminal pressure up to 200 mmHg. As they change the intraluminal pressure, SMCs may also induce nonuniform
stress distributions across the wall [123].
In summary, SMCs are very sensitive to mechanical stimuli. They tend to keep the intramural circumferential stress
as uniform as possible for physiological variations of the blood pressure, but the stress becomes nonuniform for higher
pressures [123]. They adapt their myogenic response, which ranges from 50 kPa for the basal tone under normal phys-
iological conditions to 100 kPa for maximal SMC contraction [122].
I. BIOMECHANICS