Page 415 - Advances in Biomechanics and Tissue Regeneration
P. 415
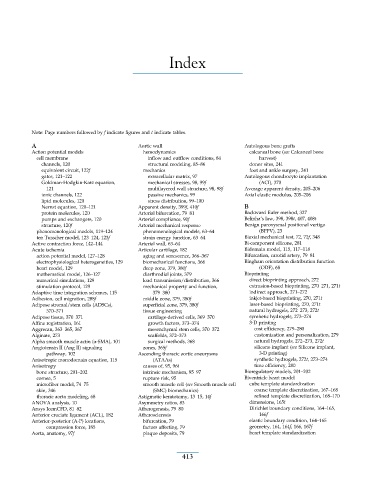
Index
Note: Page numbers followed by f indicate figures and t indicate tables.
A Aortic wall Autologous bone grafts
Action potential models hemodynamics calcaneal bone (see Calcaneal bone
cell membrane inflow and outflow conditions, 84 harvest)
channels, 120 structural modeling, 85–86 donor sites, 241
equivalent circuit, 122f mechanics foot and ankle surgery, 241
gates, 121–122 extracellular matrix, 97 Autologous chondrocyte implantation
Goldman-Hodgkin-Katz equation, mechanical stresses, 98, 99f (ACI), 370
121 multilayered wall structure, 98, 98f Average apparent density, 205–206
ionic channels, 122 passive mechanics, 99 Axial elastic modulus, 205–206
lipid molecules, 120 stress distribution, 99–100
Nernst equation, 120–121 Apparent density, 399f, 410f B
protein molecules, 120 Arterial bifurcation, 79–81 Backward Euler method, 327
pumps and exchangers, 120 Arterial compliance, 90f Belinha’s law, 398, 398t, 407, 408t
structure, 120f Arterial mechanical response Benign paroxysmal positional vertigo
phenomenological models, 119–124 phenomenological models, 63–64 (BPPV), 23
ten Tusscher model, 123–124, 123f strain energy function, 63–64 Biaxial mechanical test, 72, 72f, 348
Active contraction force, 142–144 Arterial wall, 63–64 Bi-component silicone, 281
Acute ischemia Articular cartilage, 182 Bidomain model, 115, 117–118
action potential model, 127–128 aging and senescence, 366–367 Bifurcation, carotid artery, 79–81
electrophysiological heterogeneities, 129 biomechanical functions, 366 Bingham orientation distribution function
heart model, 129 deep zone, 379, 380f (ODF), 68
mathematical model, 126–127 diarthrodial joints, 379 Bioprinting
numerical simulations, 129 load transmission/distribution, 366 direct bioprinting approach, 272
stimulation protocol, 129 mechanical property and function, extrusion-based bioprinting, 270–271, 271t
Adaptive time integration schemes, 115 379–380 indirect approach, 271–272
Adhesion, cell migration, 288f middle zone, 379, 380f inkjet-based bioprinting, 270, 271t
Adipose stromal/stem cells (ADSCs), superficial zone, 379, 380f laser-based bioprinting, 270, 271t
370–371 tissue engineering natural hydrogels, 272–273, 272t
Adipose tissue, 370–371 cartilage-derived cells, 369–370 synthetic hydrogels, 273–274
Affine registration, 161 growth factors, 373–374 3-D printing
Aggrecan, 363–365, 367 mesenchymal stem cells, 370–372 cost efficiency, 279–280
Alginate, 273 scaffolds, 372–373 customization and personalization, 279
Alpha smooth muscle actin (α-SMA), 101 surgical methods, 368 natural hydrogels, 272–273, 272t
Angiotensin II (Ang II) signaling zones, 365f silicone implant (see Silicone implant,
pathway, 102 Ascending thoracic aortic aneurysms 3-D printing)
Anisotropic monodomain equation, 115 (ATAAs) synthetic hydrogels, 272t, 273–274
Anisotropy causes of, 95, 96t time efficiency, 280
bone structure, 201–202 intrinsic mechanism, 95–97 Bioregulatory models, 201–202
cornea, 5 rupture risk, 95 Biventricle heart model
microfiber model, 74–75 smooth muscle cell (see Smooth muscle cell cube template standardization
skin, 346 (SMC) biomechanics) coarse template discretization, 167–168
thoracic aorta modeling, 68 Astigmatic keratotomy, 13–15, 14f refined template discretization, 168–170
ANOVA analysis, 10 Asymmetry ratios, 83 dimensions, 165t
Ansys IcemCFD, 81–82 Atherogenesis, 79–80 Dirichlet boundary conditions, 164–165,
Anterior cruciate ligament (ACL), 182 Atherosclerosis 166f
Anterior-posterior (A-P) locations, bifurcation, 79 elastic boundary condition, 164–165
compression force, 185 factors affecting, 79 geometry, 164, 164f, 166, 167f
Aorta, anatomy, 97f plaque deposits, 79 heart template standardization
413